What is Blood Cancer?
The term "blood cancer" is a general description of various hematopoietic cancers.

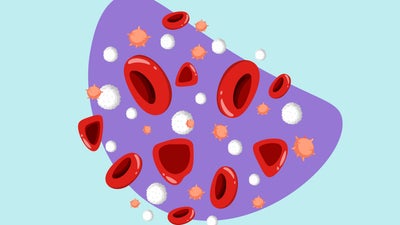
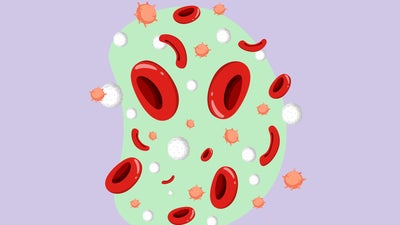
Our blood flows through blood vessels to supply all tissues in the body with nutrients. In the approximately 5 litres of blood circulating in our body there are billions of blood cells that carry out various vital functions. All blood cells originate from hematopoietic stem cells.
Haematopoietic stem cells are known as "mother cells" and do not yet have a specific function. They are able to renew and differentiate into cells with a specific function, thus replacing cells that die. In bone marrow, blood stem cells divide and develop into progenitor cells. Through further division, the progenitor cells mature and transform into different types of blood cells and then enter the bloodstream.
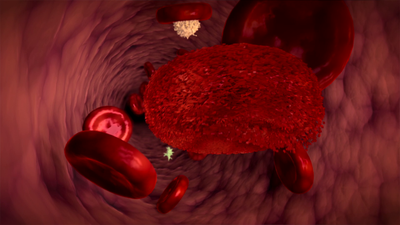
Various factors can obstruct the normal processes of maturation, differentiation and the natural dying of cells. This can lead to the formation of immature or abnormal blood cells, which enter the bloodstream and multiply in an uncontrolled way.
These immature or abnormal cells are called cancer cells. Cancer cells flood the bloodstream and drive out healthy cells. As a result, the blood can no longer perform its basic tasks, such as transporting oxygen and protecting the body from infection.